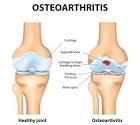
Osteoarthritis of the Knee:
The knee joint is formed by the ends of three bones: the lower end of the thigh bone (femur), the upper end of the shin bone (tibia), and the kneecap (patella). Located on the sides and in the middle of the joint are thick, non-elastic tissue bands called ligaments. Ligaments bind and connect the bones together. These ligaments also stabilize the bones so that upon movement the three bones act as a team to either transfer pressures that occur with weight bearing or allow movement within our environment. In addition to the ligaments, there are several tendons surrounding the joint.
Tendons are also thick and tough but have more of an elastic property or characteristic. Tendon is the name used to describe the attachment of muscle to bone. For example, one end of the quadriceps femoris connects the kneecap (patella) into the shin bone (tibia) and is called the infrapatella tendon (infra meaning below). Contraction of the quadriceps femoris muscle pulls on the tendon and subsequently causes the patella and tibia bone to move from a bent knee position to a straight knee position.
Often, several individual muscles will converge together to form one common tendon. In the knee for example, the quadriceps femoris is actually four muscles; the hamstring is three, two of which attach to the inside of the knee via a common tendon. Inserting into specific locations on the bone, tendons provide very efficient and specific movements within a joint. Potentially, effortless movement can be experienced when muscles are commanded to contract via an unencumbered nervous system and a normal or non-pathological joint (absent osteoarthritis, menisci or cartilage tears, ligament ruptures, etc.).
The diagnosis of Osteoarthritis (OA) is based on the presence of knee pain in conjunction with age over 50 years and/or radiographic evidence of OA (e.g. osteophytes, cysts, thinning or erosion of the hyaline or articular cartilage) coupled with other symptoms like stiffness or crepitus.1 Crepitus is the audible sound that bones make when two surfaces are in contact with each other and there is no cartilage present. Recent studies have examined age-related changes in musculoskeletal structures and walking patterns to better understand the relationship between aging and Osteoarthritis of the knee. According to Altman, et al., muscle weakness of the quadriceps femoris and joint laxity, although common in regards to healthy aging, by itself was insufficient in causing OA.2
Rudolph, et al., found that the primary difference between older adults without OA and older adults with OA, is that the two groups used very different muscle activation patterns and had specific gait characteristics. Although both groups showed quadriceps femoris weakness, the older adults without OA did not adopt a “knee stiffening” strategy (i.e. reduced knee motion and high muscle co-contraction). Common in individuals with Osteoarthritis of the knee was less knee flexion with knee adduction during peak loading of the stance leg. They compensated by increasing quadriceps activity during loading and co-contracting the quadriceps femoris and gastrocnemius (medial and lateral groups).3 For more information on osteoarthritis, see our article, What is Osteoarthritis? To understand the potential impact of Bones for Life in individual with osteoarthritis see the addendum to this article.
The Impact of Bones for Life® (BFL) and Individuals with Osteoarthritis of the Knee
There are two major active dynamic aspects in walking: “push” and “springiness.”4 The “push” is seen mostly from the foot in the rear, via the gastrocnemius-soleus (G-S) muscle group, when the lead foot makes initial contact with the ground.
In the BFL program, processes that enhance the foot organization, such as the 15. Roman Sandal, potentially have the ability to contribute to an effective “push” of the rear foot and also serve to prepare the forward foot and stance leg for its ability to transmit a domino-like pressure upward, hence, “springiness”. Since the gastrocnemius also contributes to knee flexion as well as plantar flexion in the rear foot, the 15. Roman Sandal process may play a part in restoring knee flexion in older adults with OA and perhaps even maintain knee flexion in the aging adult.
In the second aspect of walking, the “springiness” is the energy that is conserved in the non-contractile tissues (i.e. tendons) of the G-S muscle group that is being stretched as the body’s center of mass moves over the planted foot of the stance leg. Visually, this movement over the planted foot can be seen as an inverted pendulum. A person’s “springiness” is therefore also controlled by the co-contraction of muscles around a joint. When the conservation and regeneration of elastic energy is not experienced in gait patterns, such as that found in older adults with OA who demonstrate the “knee stiffening” strategy; the inherent “springiness” of a joint and the efficient and resonance seen in human locomotion, like the African Water Carriers, is lost.
The BFL program is rich in providing experiences that help a person learn and sense the stages of the gait cycle. As the nervous system becomes better informed, smooth and effective progressions, appropriate metabolic expenditure, and muscular force and co-activation occur. BFL Processes that contribute to the “push” and “springiness” of dynamic walking include 24. Knee Bends a Knee, 18. Inside/Outside Edge of Feet, 27. Sitting to Standing Spiral, 30. Jumping in the harness, 41. Distance Between the Heels, 49. Knee Straightens a Knee, 43. Functional Reflexology, 61. Bouncing on Elevation, 66. The bridge of the foot, 68. Water carriers walk #3, Creeping Series: 26., 39. and 69, 84. Heel to ischium*, 71. Ankle in kneeling*, and 72. Strategies for restoring knee function.
*Depending on the comfort level of the student in doing any of these processes, modification may be required. As a BFL teacher, particular attention should be given to the path of force as passes through the compromised knee. Reducing thehabitual deviation is the key.